The effects of the Covid-19 pandemic were felt across the globe and are still impacting us 3 years on, both in grief, economic terms, and in wider concerns for the social effects on children and education. One key group that has been found to be affected long-term by the pandemic are those over 50. In a ground-breaking collaborative research project between the University of Exeter and Kings College London, it has been shown that the effects of the social isolations in people over 50 “hold the potential for considerable detriment to cognitive and mental health, particularly because major dementia risk factors… were affected”.
Coronavirus itself, according to the Alzheimer’s Society, can worsen dementia if contracted. This is due to the side effects of delirium and “brain fog” with long Covid, or the occasion that the virus affects the brain or causes invasive ventilation treatment that may worsen confusion.
The effects of Covid-19 on dementia in this research, named the PROTECT Study, is rather due to the consequence of social isolation during the pandemic itself, through multiple lockdowns, quarantining, and social distancing. The PROTECT study is a 25 year-long longitudinal study started in 2014, investigating and monitoring brain ages and function to learn how to “reduce the risk of dementia and mental health issues in later life”.
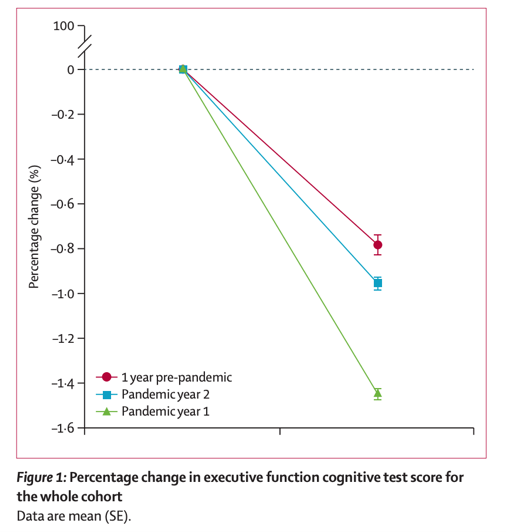
Compared to pre-pandemic data found in this study, published in the Lancet Healthy Longevity journal, it was found that: “significant worsening of executive function and working memory was observed in the first year of the pandemic across the whole cohort… in people with mild cognitive impairment… and in people with a history of COVID-19.”
Furthermore, the second year of the pandemic, even after the easing of social restrictions, also saw a persistent “worsening of working memory” and executive function with “more than a 50% greater decline” in all groups than in previous years pre-pandemic, as shown in ‘Figure 1’.
Graph to show the % change in executive function, cited from ‘Cognitive decline in older adults in the UK during and after the COVID-19 pandemic: a longitudinal analysis of PROTECT study data’
In a statement to the Guardian, the researchers stated that although the “study was observational so could not prove cause and effect but said the rise in depression, loneliness and alcohol use and fall in exercise during Covid-19 was “well known”.” In the PROTECT Study’s background summary, they state that the major dementia risk factors are “those related to exercise and dietary habits”, which were evidently affected during the two years of Covid-19 pandemic lockdowns and quarantines. More specifically, in a comment by Dr Dorina Cadar, a senior lecturer at Brighton and Sussex Medical School, who was not involved in the study, she pinpoints the major risk factors as: “reduced exercise, alcohol use, depression, and loneliness”.
In an article by Debanjan Banerjee and Mayank Rai, published in the International Journal of Social Psychiatry during the first half of 2020, the danger of loneliness, which was an observed effect of the social isolation during the pandemic, was discussed. Loneliness has been linked generally to “depression, anxiety, adjustment disorder, chronic stress, insomnia or even late-life dementia”. During the pandemic, therefore, along with the reduction of exercise due to the social restrictions on leaving the house, the decrease in physical movement was also a consequence of loneliness itself, which the article investigates:
“loneliness has also shown to be an independent risk factor for sensory loss, connective tissue and auto-immune disorders, cardio-vascular disorders and obesity. If this self-isolation and lockdown is prolonged, it is likely that chronic loneliness will decrease physical activity leading to increased risk of frailty and fractures”.
Both Banerjee & Rai and the PROTECT Study suggest changes to lifestyle in order to combat the social and physical consequences of the pandemic. As the PROTECT Study concludes, they “hypothesise that reduced exercise and increased alcohol consumption could have affected cognition”, and so, “there is a clear need to address these changes in lifestyle behaviour as a public health priority, and on the basis of the patterns of associations seen in the current study, we would hypothesise that interventions targeting these behaviours could benefit cognition”.